A BLOG ABOUT METABOLIC SYNDROME AND CUMULATIVE EFFECTS OF A POOR DIET
Gennarina Riso
 |
|
Figure 1. What if we really
looked like what we eat? I might be waddling around like a big container of
peanut butter, or even worse… a big tall beer. (http://www.mmm-online.com/mmm-awards-2011/article/214098/)
|
We’ve all heard the saying
“you are what you eat”. As well educated, young, and reasonably active
individuals, most of us don’t need to worry too much about this – we do eat
fairly healthfully on a daily basis, and even when we don’t, we have the
resources and know-how to better our food choices.
But what about people who
don’t have access to knowledge about nutrition? Since having my job in the ER,
I have thought a lot about how (seemingly) close the correlation is between
having a healthy diet, remaining active, and avoiding chronic illnesses. It
seems to me that most of the cases we see in any given day would be nonissues
if people adopted some serious lifestyle changes. In America, poor diet and
sedentary behavior are of epic proportions. And while it’s no news to us that
being chronically overweight and eating a typically high-fat Western diet contribute
to incidence of Type II Diabetes, high cholesterol, and high blood pressure
(just to name a few), the cumulative effects of having a poor diet are much
more convoluted and additive than they appear. But how many people truly
understand what lifestyle choices to make? And further, can they afford to do
so?
In addition, I got to
thinking about how exactly Americans became so unhealthy – what is it about our
society in particular that leads to such overabundance of excess? According to my
research, much of the “spike” in obesity in this country is due to the
increased availability of meat and oil products after World War II (not to
mention plastic and other conveniences). In addition, the concept of “super
sizing” or “economy sizing” (in other words, getting more product for less
money) played greatly into the spike in calorie consumption that took place.
Families who once barely had enough food or resources to survive could now buy
more food than they could ever dream of, so self-control was really not at play
here, and with good reason. In addition, where families once made their own
food from scratch, grew their own vegetables, and owned one family car,
suddenly streamlined products appeared on the market that greatly changed the
dynamics of the American household. Suddenly, America was more focused on
productivity than ever – and while there are thousands of such examples, TV
dinners are particularly symbolic in terms of this topic, as cooking and eating
meals together became less common than heating up a frozen meal in the
microwave and sitting in front of the television.
 |
|
Figure 2. An example of a
classic Swanson TV dinner from the 1950’s. Very convenient, but how much
nutritional benefit is there? (http://itthing.com/the-history-of-the-tv-dinner)
|
But what is it exactly about
eating poorly that contributes to such physiological mayhem down the line? And
how is it that our diet can play into our immune function and cause inflammation?
The answer is surprisingly
straightforward, as I learned this quarter in BMED 545. When the endothelial
cells that line our blood vessels become activated (which can happen in
response to turbulent blood flow, or even simply increased blood flow), they
express adhesion molecules that allow monocyte extravasation into the
subendothelial space. They also secrete chemokines (such as MCP-1) that help
activate leukocytes. So, when macrophages are present in the subendothelial
space, they secrete cytotoxic superoxides in order to prevent infection. If
there are high plasma LDL levels, once they filter through the space between
contracted/activated endothelial cells, they react with these superoxides,
which is a very bad situation, as this contributes to the positive feedback
loop that involves more and more immune activation and eventually leads to the
formation of a plaque that contains cholesterol, LDLs, macrophages, and other
immune cells (such as helper T cells, which secrete INF-g, causing macrophages to secrete TNF-a, both
of which are common proinflammatory markers). Obviously plaque formation alone
is dire, but if that plaque ruptures, endothelial cells are exposed to many
combinations of factors that can lead to a blood clot quite easily, most commonly
leading to MI, but also seriously increases risk for stroke and pulmonary
embolism.
 |
|
Figure 3. A simple schematic of how eating a
poor diet can lead to coronary heart disease (CHD), just to name one deleterious
side effect.
|
As if all of this isn’t scary enough, research
has shown that increased emotional and psychological stress can promote some of
the oxidative and proinflammatory pathways (even in the absence of physical
injury) that having a high fat diet can – so imagine how dangerous it would be
to be stressed and eat poorly! Because depression is also correlated with poor
sleep patterns, which further increase our risk for infection and immune
response, it is easy to see how this situation could spiral out of control. Janice
Kiecolt-Glaser (2010) cites longitudinal studies that explicitly show that
people who are chronically stressed over a 6 year period have significantly
higher amounts of proinflammatory cytokines circulating through their bodies at
a given time than those without chronic stress. Further, postprandial lipemia
can also increase expression of inflammatory markers, and while the spike in
lipid levels may be short-lived, the positive feedback loop associated with
some of this inflammation could be much longer lasting and cumulative,
especially if a high fat diet is the “norm”. Similar research also indicates
that one single meal high in fats can lead to endothelial cell activation and
increased expression of adhesion molecules that are necessary for the monocyte
extravasation that I mentioned above.
 |
|
Figure 4. Even the autonomic nervous system is involved!
Although, that is a subject for another day.
|
Before I begin to talk about some of the ways
we can combat having metabolic syndrome ourselves, I just have to share one
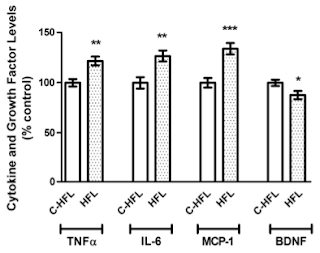
more thing… Pistell et al. (2010) performed fascinating study using a mouse model
that showed that mice who were fed a high fat diet (in particular, a “high lard
diet”) showed cognitive impairment when compared to mice who ate a regular
diet. Further, these same mice were also shown to have significantly higher
levels of proinflammatory markers in their brains (Fig 5)! If that won’t make
you stop hitting up Jack in the Box, I don’t know what will.
 |
|
Figure 5. Mice fed a high-fat lard diet showed
significantly higher levels of the above mentioned proinflammatory cytokines
and markers when compared to mice fed a control diet.
|
The good news? As discussed in BIO 502 lab last
week, eating a Mediterranean Diet has been associated with lower instance of
heart disease and many of the pathologies I described above. In 2011, Kastorini
et al. did a metanalysis on 50 past studies involving the Mediterranean Diet
(MD) and metabolic syndrome, and they showed that not only is the MD negatively
associated with metabolic syndrome as a whole, but also with all of its
separate components! Luckily, eating like an Italian is no punishment; all you
have to do is eat a well-balanced diet of fruits, vegetables (flavonoids!),
whole grains, healthy fats (olive oil!) antioxidants (salmon!), and even some
dark chocolate and red wine. They key to adopting the healthy Mediterranean
style is moderation. For example,
studies that show lower instance of heart disease, obesity, inflammation, and
high cholesterol in people who comply with a MD also note that they have a
relatively lower dairy intake than a Western Diet, and the dairy that they do
consume is generally low-fat. After all, we must take into account inflammation
in the animals we consume and how that may manifest in our own bodies. But that
is a subject for another day.
Essentially, the take-home message is that our
grandparents and great-grandparents would have been better off (I will argue)
from a health perspective if they did not change their dietary habits in such a
drastic manner.
 |
|
Figure 6. A Mediterranean Food Pyramid. Note
that it gives you information about what you should be consuming on a daily,
weekly, or monthly basis! (http://pikimal.com/diet/vs/dash-diet/mediterranean-diet)
|
Mangiate, bevete e sopratutto divertitevi!
(Eat, drink, and be merry!) In moderation, of course; at least in regards to
the eating and drinking J
 |
|
|
References
Pistell, P., C. Morrison, S. Gupta, A. Knight,
J. Keller, D. Ingram, and A. Bruce-Keller. 2010. Cognitive impairment following
high fat diet consumption is associated with brain inflammation. Journal of
Neuroimmunology 219:25 – 32.
Nicklas, B., W. Ambrosius, S. Messier, G.
Miller, B. Penninx, R. Loeser, S. Palla, E. Bleecker, and M. Pahor. 2004. The
American Journal of Clinical Nutrition 79:544 – 551.
Giugliano D., A. Ceriello, and K. Esposito.
2006. The effects of diet on inflammation. Journal of the American College of
Cardiology 48:677 – 685.
Esposito, K., and D. Giugliano. 2006. Diet and
inflammation: a link to metabolic and cardiovascular diseases. The European
Heart Journal 27:15 – 20.
Chrysohoou, C., D. Panagiotakos, C. Pitsavos,
U. Das, and C. Stefanadis. 2004. Adherence to the Mediterranean Diet attenuates
inflammation and coagulation process in healthy adults. Journal of the American
College of Cardiology 44:152 – 158.
Kastorini, C., H. Milionis, K. Esposito, D.
Giugliano, J. Goudevenos, and D. Panagiotakos. 2011. The effect of
Mediterranean Diet on metabolic syndrome and its components. Journal of the
American College of Cardiology 57:1299 – 1313.
Alberti, K. and J. Shaw. 2005. The metabolic
syndrome – a new worldwide definition. The Lancet 366:1059 – 1062.
Kiecolt-Glaser, J. 2010. Stress, food, and
inflammation: psychoneuroimmunology and nutrition at the cutting edge.
Psychosomatic Medicine 72:365 – 369.
Physiological Mayhem! Great post Gennarina
ReplyDelete